I thought I’d earned a reprieve from the hospital grind. After all, my November ordeal felt like more than enough to last a lifetime. But cancer, as I’ve learned, has its own plans—and they rarely involve taking it easy. So there I was, back in my oncologist’s office, determined to avoid the chemo drugs that had wreaked havoc on my immune system and left me so anemic I’d needed a transfusion to stay upright.
Chemo, it turns out, isn’t just tough on cancer—it’s tough on everything else too. Sure, it’s effective at shrinking tumors, but it also comes with side effects that range from “slightly annoying” to “potentially life-altering.” Cyclophosphamide, one of the drugs in my regimen, carried the risk of early-stage interstitial lung disease—a complication I wasn’t keen to roll the dice on.
When I voiced my concerns and my reluctance to continue, my oncologist gave me a look somewhere between worry and polite disbelief, as though she was weighing whether I was being overly dramatic. But I was firm. That last hospital stay had been a wake-up call. I wasn’t willing to put myself through that again if there were alternatives.
After a pause, she leaned forward with a new plan. “What if,” she said, “we could do surgery earlier? If your surgeon agrees, and we don’t find any evidence of cancer, you could skip the final three chemo treatments.”
Now that was a proposal I could get behind. My tumours had already done me the courtesy of shrinking, so all I needed was a lumpectomy and a lymph node dissection. One night in the hospital, tops.
Enter my superhero surgeon, who swooped in with a December 19th surgery date. Yes, my wedding anniversary! Nothing says “romance” like hospital gowns and anaesthesia, right? But hey, the timing felt poetic: celebrating love and fighting for life all in one day.
December 19th arrived, and I found myself heading into the hospital, bracing for what they kept referring to as a “small surgery.” I used the term loosely—after all, when a procedure involves wires, lymph nodes, and a surgeon reworking your internal layout, it doesn’t exactly feel minor. Still, I was ready. Nervous, absolutely, but ready.
The day began with registration, where I opted for a semi-private room. With my immune system still recovering, a little extra space between me and potential sources of infection seemed like a worthwhile investment. After that, it was off to Day Surgery to slip into one of those universally unflattering backless hospital gowns. It wasn’t exactly comfortable, but by now, I’d resigned myself to the peculiar uniformity of hospital wear.
With vitals checked and the usual pre-op questions answered, it was time for the part I’d been dreading: radiology. Here’s where things took an unexpected turn. The radiologist and technician explained the process, involving a mammogram machine and guided wires. The goal was to pinpoint the tiny metal markers left behind from my biopsy, which would direct the surgeon to what was left of my tumors. The explanation made sense, but the idea of being wired up like a human antenna was less than comforting.
Delightful, right?
The mammogram machine—a device I already had little fondness for—was back in action, this time to position the wires with precision. It was an odd and slightly uncomfortable experience being smooshed into the machine, but I knew it was necessary. Those markers, reduced to GPS coordinates for my surgeon, represented both how far I’d come and the final hurdle ahead.
The plan? The surgeon would remove the mushy tissue around the metal pieces, do some internal redecorating to make it look like she’d never been there, and then tackle the lymph nodes. Easy-peasy, right? Well, at least I hoped so. Because by then, I’d had just about enough of being poked, prodded, and wired for one day.
Despite the strangeness of the procedure and the weight of the day, I reminded myself that this was one more step toward healing. It wasn’t easy, but I was determined to see it through.
Lately, it feels like every time I step into a hospital, Murphy’s Law is waiting to escort me through the door. If there’s a complication to be had, I somehow manage to find it. Case in point: during or shortly after what was supposed to be a “routine” surgery, my right lung decided to go rogue and collapsed. A pneumothorax, they called it—medical jargon for “your lung threw in the towel.”
The real kicker? No one realized what had happened for two full days. At first, the signs were subtle but unnerving. The day of surgery, I felt like I’d been hit by a freight train. Lightheaded? Definitely. Walking in a straight line? Not a chance. Even shuffling a few feet to the bathroom left me gasping for air like I’d just run a marathon. I wondered, “Is this anemia acting up? Low red blood cells? Or am I suddenly incapable of basic human functioning?”
When my surgeon came by for her rounds, I made my case. “I don’t think I’ll make it up the stairs at home. Can I stay one more night?” She hesitated—probably assuming I was being overly dramatic—she hesitated, but agreed. Her reluctance wasn’t exactly comforting, but I was grateful for the extra time.
That extra night, the nurses kept a close eye on my oxygen levels, which hovered far below where they should’ve been. By the next morning, my surgeon returned with a new condition for discharge: “You can go home if your oxygen levels stay above 92%.” It sounded reasonable in theory, but my body apparently didn’t get the memo. The nurses monitored me closely, their increasingly concerned faces making it clear something wasn’t adding up.
By that evening, the tension ramped up. My night nurse popped in and out of my room so often, I half-expected him to start leaving personal belongings behind. Every time he checked the pulse ox levels, his expression grew more serious. Meanwhile, I lay there, grappling with the sense that something was very wrong, even if I didn’t fully understand what. Confidence was not exactly abundant.
It wasn’t until much later that the collapsed lung revelation came to light. Classic me—turning a routine hospital stay into a medical mystery. If only I could channel this level of unpredictability into something fun, like winning a lottery, instead of starring in episodes of When Lungs Attack.
When my surgeon walked in on the fourth morning, the surprise on her face was unmistakable, as if she hadn’t expected to see me still there at all. But her real shock came when she noticed my oxygen levels, which were still playing limbo—how low can you go? Off I went for an X-ray, where they finally discovered the culprit: my lung had decided to pack it in and collapse. A pneumothorax. Lovely.
And so began the saga of the chest tube.
Now, I’ve come a long way from my days of fainting at the mere thought of a needle or blood. Years of pokes and prods have desensitized me—or so I thought. But the idea of a tube snaking its way into my chest and nestling up against my lung? Nope. That’s nightmare fuel. They assured me it would be fine because, well, they’d pump me full of drugs like a guest of honour at a pharmaceutical party. They weren’t wrong—I barely remember the procedure—but boy, did I feel it after.
Once the tube was in, the real fun began. It found a nerve to cozy up against, sending searing pain into the front of my shoulder and right through to my shoulder blade. It was the kind of pain that makes you want to ask, “Who ordered this feature?” Enter the opioids, my uninvited but very effective party guests.
For the next few days, I was floating somewhere between reality and a cloud of chemically induced euphoria while my lung slowly reinflated. Sure, I was in agony, but at least I was high enough to find it all mildly hilarious. If there’s a silver lining to a collapsed lung, it’s that you’ll get a front-row seat to the weird and wonderful world of modern medicine—whether you want it or not.
The days dragged, inching past Christmas Eve, Christmas Day, and Boxing Day as if time itself were stuck in the hospital’s dreary fluorescent glow. Determined not to dampen everyone else’s celebrations, I sent my husband off to my son’s house for Christmas Eve. Thanks to the miracle of video chat, I got to join in virtually, catching glimpses of the family and their festivities from my hospital bed.
Christmas Day was quieter—just my husband and me in that little room. My daughter-in-law saved the day, though, with a video call that included the two youngest grandchildren gleefully showing off their gifts. Seeing their joy made the day feel a bit brighter. On Boxing Day, one of my daughters sent over two turkey dinners for us, which we enjoyed together in my room. Then we video chatted with her family and even exchanged gifts remotely. It was a new kind of Christmas—unconventional, but still filled with love.
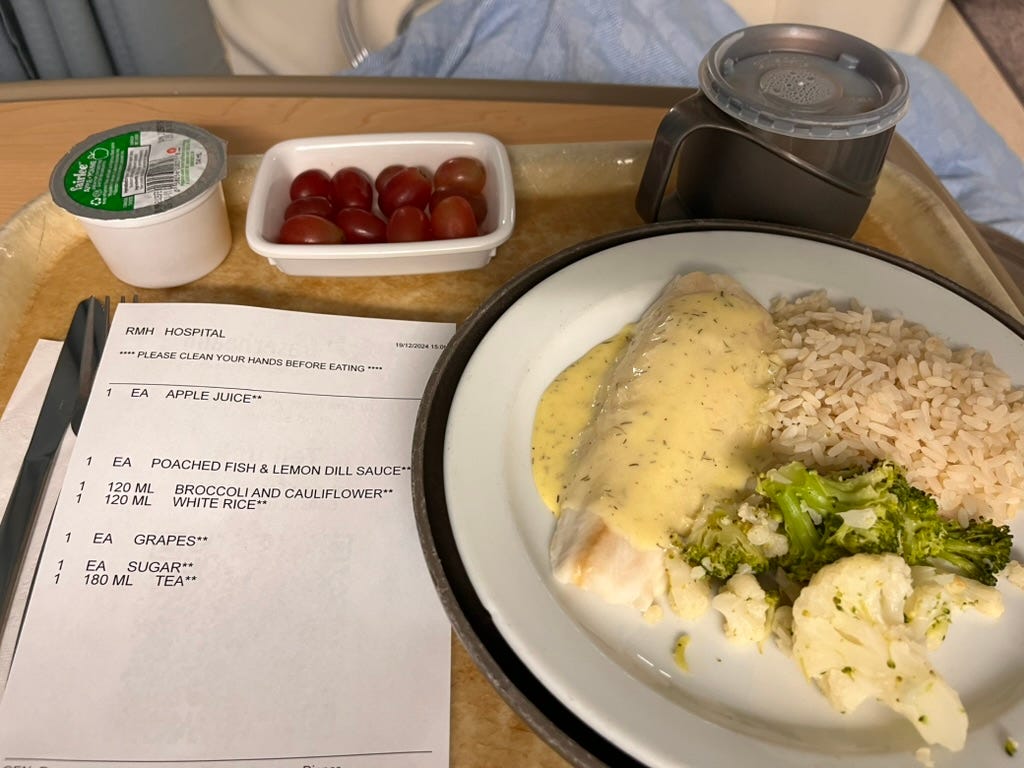
What wasn’t filled with love? The hospital food. Gluten-free options meant my choices were limited, and what I did get was as dry and lifeless as my enthusiasm for another PB&J sandwich. (Which, by the way, used to be my favourite—past tense.) My first “real” hospital meal was dry fish with dill sauce, and let’s just say the sauce was the only thing carrying the team.
Thankfully, my daughter cooked up some delicious meals and sent them over, giving me something to actually look forward to during my stay. Her efforts made the days a little easier to bear. Because honestly, if you can’t rely on good food, what else is there?
In the end, my “quick” hospital visit turned into a 10-day saga. And then it hit me: I’d been paying extra for that semi-private room all along! At this rate, I could’ve upgraded to a luxury suite—if such a thing existed in hospitals. Thankfully, they only billed me for a ward—small mercies in the world of hospital surprises!
Throughout my hospital stay, I clung to prayer like a lifeline, hoping and pleading for healing to come swiftly. Fear crept in like an unwelcome guest, stronger than anything I’d experienced before—even more than during my November ordeal. This was different, more consuming. Would my lung reinflate? Could this lead to other complications? How long would it take to fully recover? Would there be permanent damage? My mind swirled with questions I couldn’t answer, and as much as I tried to stay calm, the worry was hard to push aside.
“When I am afraid, I put my trust in you.”
– Psalm 56:3
I leaned on my faith as best I could, though there were moments when holding onto it felt like trying to grasp water. Without the unwavering support of my best friend and my Friends in Prayer group, I don’t know how I would have managed. Their prayers, their words of encouragement, and their constant reminders of hope became a source of strength that carried me through those uncertain days.
“God is our refuge and strength, an ever-present help in trouble.”
– Psalm 46:1
Each prayer, every positive thought, every message of support, and every funny video felt like a light piercing the shadows of fear. It reminded me that I wasn’t walking through this alone, that there was a greater power at work, and that healing, in its time, would come.
As I wait for the pathology report to reveal the next steps in this cancer journey, I’m struck by how fragile our hold on life can be. This season of waiting has brought a surprising gift: a deeper appreciation for the small, often-overlooked moments that make up our days. The beauty in everyday encounters—the kindness of a stranger, the warmth of a familiar face, the quiet rhythm of ordinary life—feels more vivid now.
I find myself looking at others and wondering about their struggles, their fears, the challenges they might be quietly carrying. I’ve always been a compassionate observer, but now it feels more profound, more personal. This change, this heightened awareness, is something I welcome. It reminds me to slow down, to stay grounded in the present, and to resist the pull of worrying too much about what lies ahead. Life, after all, is best lived one day at a time.
To you, dear readers, you who’ve been walking this journey with me, I send a belated Merry Christmas and Happy New Year. My hope and prayer for 2025 is that it will be a year where you too find wonder in the small, ordinary moments of your lives. May you learn to embrace the present, and may the weight of life’s worries lift as you navigate your own path with grace and hope. Bless all of you.
With much love and gratitude,
Kathie
PS. I am home now and doing much better. My oxygen levels are improving and I was able to venture out to the oncologist on my own.








Your writing is so beautiful, Kathie, and your wit and humour are a miracle in the light of such challenging times. Despite those hours with persistent low oxygen, your brain has come through unscathed. Not to press too hard on the lung puns, but you are owed a little breather from your medical ordeals, and I add my prayers to all the others in your support that you will get one.
You write in a way that makes me feel I am with you. Remember that over lonely times. I hope you continue to feel God's presence too--the God who suffers for and with the suffering.